- #1
Graham87
- 70
- 16
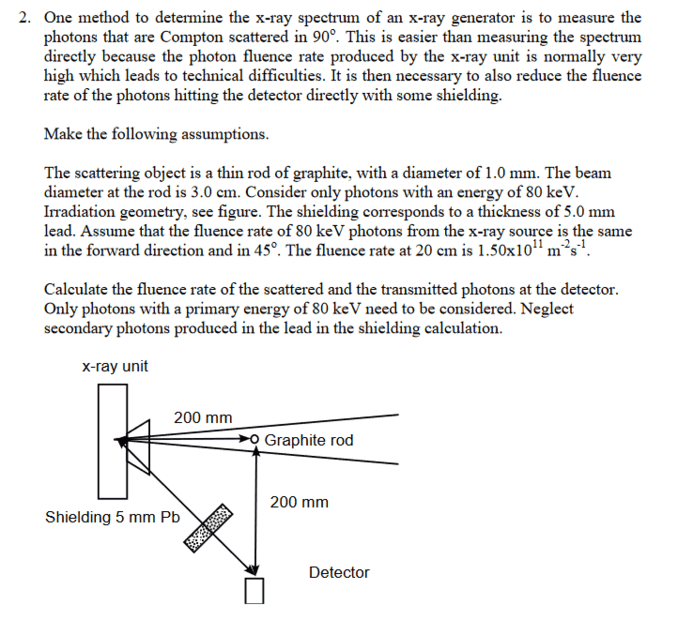
- Homework Statement
- See pictures
- Relevant Equations
- See pictures
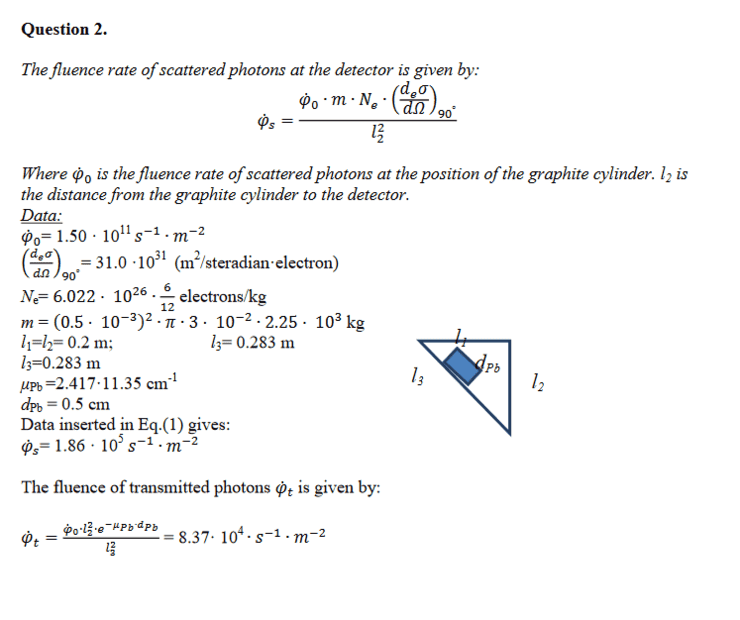
I managed to calculate the fluence of the scattered photons. However, not the transferred photons. In the solution sheet the fluence rate has an l22 in the numerator in the end of the solution sheet. Where does that come from?